Multi-Agency Pre-Birth Wellbeing Assessment for Unborn Babies
Scope of this chapter
All prospective parents are offered a universal health service in the form of antenatal care from their registered GP, Obstetrician, Midwifery and Health Visiting Services (please see Gov.Je Information). Health services are offered to all parents throughout pregnancy and birth. All children have an allocated health visitor from pre-birth to 5 years of age. Health services do not work in isolation and work in partnership with other services. In relation to taking action to safeguard the welfare of an unborn baby, no practitioner or agency should assume midwifery or local health services are aware of a pregnancy or the needs/vulnerabilities of prospective parents. This practice guidance outlines the responsibility all practitioners have in recognising wellbeing, health and development and safeguarding needs, with guidance on the actions that must be taken to protect the unborn baby's health, development and welfare.
All practitioners must be aware of their individual and collective Roles and Responsibilities in identifying and taking action when they identify wellbeing, health and development needs and safeguarding the welfare of children (see SPB Jersey Roles and Responsibilities Procedure).
All practitioners must understand Capacity, Consent and Safeguarding Young People (see SPB Jersey Introduction Procedure).
This practice guidance advises services to take a collaborative, sustained approach throughout the antenatal period and post-delivery, rather than a 'stop-start' approach where there are long periods of time where no work is being undertaken. Identifying need at the earliest possible point in pregnancy reduces the likelihood of late or unplanned activity around the time of birth, which can cause unnecessary distress to prospective parents/carers.
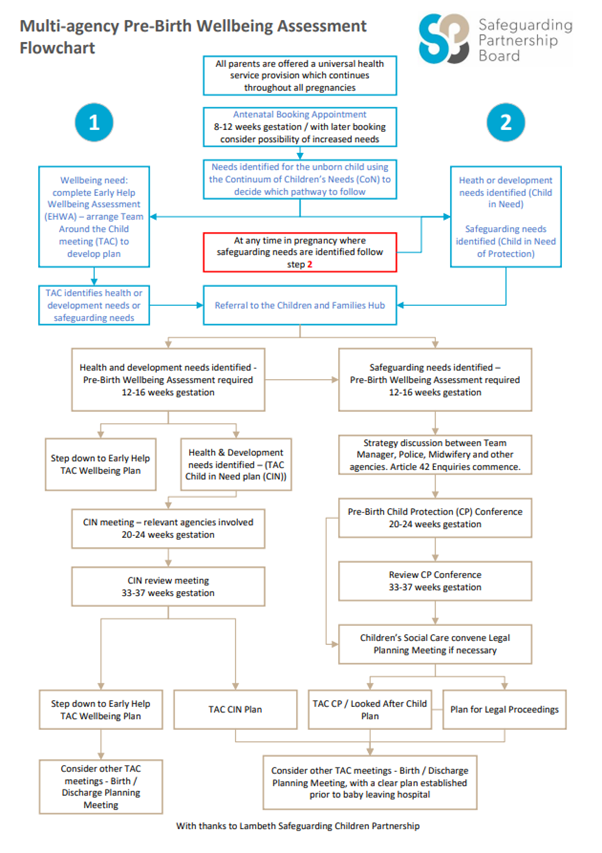
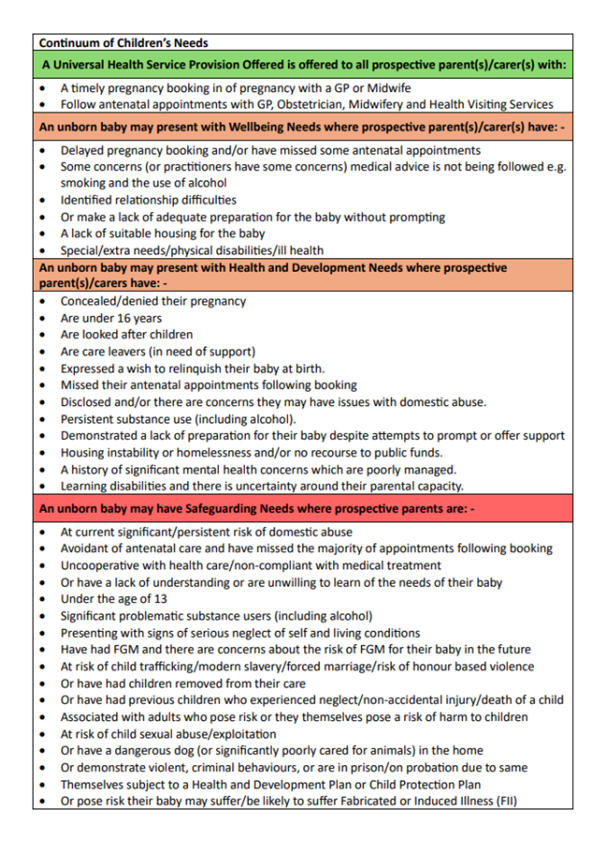
Practitioners are advised to use the Continuum of Children's Needs (CoN) to support their decision-making. They should follow this practice guidance to help them identify when an unborn or newborn baby may require more than a universal health service provision. Such as an Early Help Wellbeing Assessment (EHWA). Support with their Health and Development needs (Child in Need of support) or Safeguarding Needs (Children in Need of Protection), (see SPB Jersey Multi-Agency Flow Chart, and Appendix 1).
Amendment
In September 2025, this chapter was amended to align with the Children and Young People (Jersey) Law 2022 and commensurate statutory guidance. This chapter includes information on the use of the Jersey Children’s First Framework, Single Agency Supervision and the use of Professional Difference/Escalation.
The most significant updates relate to wording which discusses assessing strengths and needs, and where required risk, with recommendations that all practitioners use the Islands Continuum of Children’s Needs (CoN) (2024) to support their decision making.
There is an updated multi-agency flow chart (which has had multi-agency agreement from Health, Children’s Social Care, Children and Families HUB and FN&HC). The flow chart has a quick link guide with the pre-birth information in the CoN.
This practice guidance adds safeguarding indicators for practitioners on identifying risks associated with links to SPB Jersey Chapters which were updated in 2024 and 2025 around pregnant children under the age of 13, disclosure of child sexual abuse or child exploitation, modern slavery, child trafficking, forced marriage, dangerous dogs, Fabricated and Induced Illness (FII) (these are of relevance and are not currently in the islands CoN).
Further information was added with updated publications from the Child Safeguarding Review Panel, NSPCC and Nice Guidelines focusing on the importance of working with and including fathers/ carers in assessments of need and on the need to assess for risks associated with Sudden Unexpected Death in Infancy (SUDI), with the advice on how to assess for risks and what steps to take to reduce these using the islands SUDI Assessment Tool Kit included in the islands Neglect Strategy.
Timescales were remained unchanged, and we have a multi-agency agreement and are in line with SPB Jersey Core Child Protection Procedures.
Unborn babies are among the most vulnerable individuals we work with. Research such as Dickens et al (2022), Triennial Analysis into Serious Case Reviews, reminds us that effective work in the antenatal period can significantly reduce the likelihood of harm. Early assessment, meaningful engagement and timely intervention make a difference, and this work starts with forming trusted relationships with families. Where the antenatal period offers a unique opportunity to understand the world into which a child will be born.
Practitioners in Jersey are encouraged to take a 'Think Baby, Think Family' approach, working alongside families to:
- Build early relationships, centred on the unborn baby's wellbeing;
- Identify vulnerabilities and risks early;
- Understand how parental needs and circumstances may impact them;
- Explore collaborative safety planning;
- Assess parenting capacity and protective factors in preparation for birth;
- Make appropriate referrals and undertake assessments, including Early Help Wellbeing Plans and Pre-Birth Wellbeing Assessments;
- Coordinate multi-agency planning and communication;
- Support legal planning where required, including the Child Protection Pathway and Pre Proceeding processes;
- Ensure that no child waits unnecessarily for care and protection where thresholds for significant harm are met.
The principles of personalised, relationship-based practice, as advocated in the National Maternity Review: Better Births (2016), remain relevant in our local context. Actions must be responsive to the lived experience of the baby and the wider family. The importance of conducting a timely Pre-Birth Wellbeing Assessment has been highlighted by numerous research studies (Research in Practice). Babies identified as needing Pre-Birth Wellbeing Assessment but who did not receive one have been found to be at the greatest risk of significant harm and fatality within the first year of life, (NSPCC Learning from Serious Case Reviews and Serious Case Review in relation to Clare and Ann.
While most pregnancies do not raise safeguarding concerns, it is crucial that when vulnerabilities are identified, services respond with compassionate curiosity and coordinated action. Working in a small island context like Jersey requires thoughtful attention to relationships and the importance of joined-up support.
This practice guidance aims to enable practitioners to work together with families to safeguard unborn babies where risk is identified (this practice guidance holds relevance for newborn babies where SPB Jersey Core Child Protection Procedures must be followed).
This practice guidance establishes a shared process for response, with an emphasis on clear, timely, and regular communication between professionals supporting the pregnant person and their wider family, which is agreed across the Safeguarding Partnership Network including health agencies, children and adults social care, police and other key partners involved in Pre and Post Birth Wellbeing Assessment, planning and delivery of support to safeguard unborn and newborn babies.
The antenatal period and the child's first five years of life are extremely important, as this is where the foundations of physical, emotional, and social development and attachments are laid (Bowlby 1969, cited in McGarvie 2024). Where the child's relationship with their parents/carers shapes their physical, emotional and future wellbeing, health and development. Adverse childhood experiences (ACEs) may start before babies are born www.beginbeforebirth.org. If an unborn baby is exposed to substances, alcohol and stressors such as domestic abuse during pregnancy, these pose the risk of lifelong negative impacts. These risks may be reduced with early interventions, supporting prospective parents/carers with their use of substances (including alcohol), working with them to improve their home environments and their mental and physical health. Understanding needs and offering support to improve prospective parents/carers' social circumstances, networks and relationships can reduce their anxiety and prepare them for the birth of their baby. This has the potential to improve their baby's health outcomes greatly. Multi-agency action taken to safeguard the welfare of unborn babies and support prospective parents in pregnancy has the potential to improve the long-term well-being, health and development of children. Whilst reducing the risk of future health problems related to foetal alcohol/abstinence syndrome, sudden infant death, abuse and neglect.
In Jersey, effective safeguarding of children and young people relies on timely and appropriate information sharing. All practitioners have a legal and professional duty to share information where necessary to promote the welfare and protect the safety of children (see SPB Jersey Introduction).
Practitioners must be familiar with and act in accordance with the CYP Law 2022 commensurate Statutory Guidance on Information Sharing, which supports multi-agency working and a child-centred approach to decision-making (see also Data Protection (Jersey) Law 2018).
The terms mother, father and prospective parents/carers are used to describe persons in this role.
In order to remain neutral, this protocol will refer to "the person who has given birth to the child," "the pregnant person," or the "person."
The Antenatal Period - commences at the start of pregnancy and continues to the onset of labour.
Antenatal Care - The maternity care received by persons during pregnancy. This can also be called pregnancy or maternity care.
Concealed Pregnancy -This is a situation where the pregnant person is aware they are pregnant, however, conceals the pregnancy from family/friends and/or health practitioners. The reasons for concealment and lack of engagement can be varied; however, they should always initially present as a safeguarding concern and are identified risk factors for potential significant harm.
Expected Date of Delivery (EDD) - The date a baby is due to be born. Prospective parents will normally be given their baby's EDD by their Midwife, following their first antenatal appointment.
Gestation - The term gestation is used to describe the weeks of a pregnancy. A normal pregnancy ranges from conception to between 38 and 42 weeks of gestation. Infants born before 37 weeks of gestation are considered premature, and infants born after 41 weeks of gestation are considered late term.
Strategy Meetings/Discussions, Article 42 Enquiries, Initial Child Protection Conference (ICPC), Review Child Protection Conference (RCPC's), Core Group Meeting (CGM) - describe Jersey's Core Child Protection Procedures (where further information on each of these topics can be found as well as Practice Guidance on other specific related issues).
Each prospective parent/carer will be unique in the level of support they require, and it is important to assess the strengths and vulnerabilities of both prospective parents/carers. The role and importance of fathers is further discussed below, see Further Information.
The aim of a Team Around the Child (TAC) Early Help and Pre-Birth Wellbeing Assessments is to identify need and offer timely supportive responses to prospective parents/carers. The Lead Worker who offers prospective parents an Early Help Wellbeing Assessment may come from several different agencies.
The Lead Worker undertaking a Pre-Birth Wellbeing Assessment will be the unborn baby's allocated Children's Social Worker (CSW). The allocated lead worker will coordinate a TAC Process (see JCF) and consider the plan of care required to meet the well-being, health, development and safeguarding needs of the unborn baby (please see SPB Jersey Assessment).
Research demonstrates parental motivation to change is at its highest during the antenatal period (Lindqvist et al, 2017, Research in Practice Pre-Birth Assessment. The antenatal period provides a window of opportunity and the time prospective parents /carers need to have the best possible opportunity to prepare for the birth of their child.
It allows them to:
- Form relationships with trusted professionals;
- To focus on their wellbeing and health needs, which helps them to prepare for their unborn baby and understand how to meet their wellbeing, health and development needs;
- Look at the practical support they may require with finances and housing (it is important to note that those who have been on the island for under a year may incur costs when they give birth, see Doctors (GPs) fees, prescriptions and health cards).
It allows practitioners to:
- Assess strengths and needs across all 8 wellbeing indicators within the JCF's model of practice and assessment (this may lead to the evaluation of risk);
- Explore and agree on health and safety planning options;
- Assess parental capacity to parent their baby when they are born;
- Consider family group conferences to understand supportive networks;
- From a team around the unborn child to support prospective parents/carers before their baby is born;
- Develop a wellbeing plan to enable the wellbeing, health, development and safeguard the needs of the unborn child;
- Enable safety and care planning and the provision of ongoing care and support at birth and into childhood;
- Referral to supportive services such as Adult Social Work, Drug and Alcohol, Adult Mental Health and Parenting Support and consideration for Parenting Assessment, for example, Parent Assess;
- Ensure all assessments are undertaken to inform decisions regarding the child's safeguarding needs will be met. This may take place under the process of pre-proceedings before the birth of the baby.
The Health Safeguarding Team and Safeguarding Midwife Advisor work in partnership with GPs, Health Visiting Services, Family Support Services and Adult Services, where they coordinate services based on the identified needs of prospective parents/carers from initial booking throughout the antenatal period and post-delivery.
Referrals to supportive services should happen as early in pregnancy as possible around 8 - 12 weeks gestation, (or at any time need arises) and should continue for as long as required (See Pre-Birth Wellbeing Assessment Flow Chart and Appendix 1). Taking into consideration late bookers and those prospective parents who may present at any time in pregnancy with indicators of need (see CoN).
Pro-active referrals should be made for prospective parent(s)/carer(s) to:
- Antenatal classes such as Baby Steps, Brighter Futures - Brighter Storks;
- Health Visiting Services and their Maternal Early Childhood Sustained Home Visiting (MECSH) Programme, where there is an identified need for extra support.
Or specialist health and supportive services (which include not only the pregnant person but also, where required, their partner) to:
- Mental Health Services;
- Alcohol and Drug Services;
- Jersey Domestic Abuse Services (JDAS) and FREEDA.
This list is not exhaustive. In accordance with the JCF model of practice, it is important to make referrals to supportive services as soon as needs are identified to ensure all relevant partner professionals are part of the team around the child.
When considering need, it is important to consider not only prospective parents/carers but also frequent visitors to the family home who may provide a caring role. Practitioners should share their assessment of strengths and risks with prospective parents/carers to gain their understanding, unless in doing so the unborn baby, any siblings, a pregnant person or others are found to be at an increased risk of significant harm by doing so.
Parents/Carers may present with multiple indicators of need, some of which may be assessed as wellbeing needs, some as health and development needs, and some as Safeguarding Needs. Where this is the case, practitioners should use the CoN to assist in their decision making.
TAC Early Help - Where practitioners anticipate prospective parents/carers may need support to meet the wellbeing needs of their unborn baby and/or baby at birth, they should offer a JCF Early Help Approach, (see JCF - Early Help), begin an Early Help Wellbeing Assessment (EHWA), arrange a TAC Meeting to develop an Early Help Wellbeing Plan (EHWP) (see SP Jersey Multi-Agency Flow Chart and Appendix 1).
The following indicators may trigger an EHWA:
- Delayed booking in for pregnancy and/or are missing antenatal appointments.
- Parental (or practitioner) concern that medical advice cannot/or is not being followed, e.g. smoking, use of substances (including alcohol).
- There is disclosed or identified relationship difficulties.
- A lack of suitable housing for the baby.
- Parent/Carer(s) learning/physical disabilities/ill health.
TAC Wellbeing Assessment for Health and Development Need (CiN) - This is not an exhaustive list, where prospective parent(s)/carer(s) present with or the practitioner assesses, indicators of health and development need, this must trigger referral to the Child and Family Hub for consideration of a Pre-Birth Wellbeing Assessment.
Prospective parent(s)/carer(s) who:
- Have concealed/denied pregnancy;
- Are under 16;
- Are looked after children;
- Are care leavers (in need of support);
- Have expressed a wish to relinquish their baby at birth;
- Have missed the majority of antenatal appointments following booking;
- Experiencing or has experienced Domestic Abuse;
- Have problematic substance use, which includes alcohol;
- Demonstrate a lack of preparation for their baby despite attempts to prompt/offer support;
- Have housing instability or homelessness and/or have no recourse to public funds;
- Have a history of mental health concerns which is poorly managed;
- Have learning disabilities (and in some circumstances those who may have severe physical or mental disability) and there is uncertainty around their parental capacity to meet the needs of their baby once born, (see SPB Jersey Children of Parents with Learning Disabilities);
- There may be presentation of multiple indicators of need, some may present as wellbeing needs and others as health and development needs, where this is the case, refer to the CoN to help in the assessment of need.
This is not an exhaustive list, but where prospective parent(s)/carer(s) present with, or the practitioners assess indicators of safeguarding need, this must trigger referral to the Child and Family Hub for the consideration of a Pre-Birth Wellbeing Assessment.
Prospective Parent(s)/Carer(s) who:
- Have current significant or persistent issues with domestic abuse (see SPB Jersey Domestic Abuse Procedure);
- Avoid antenatal care, missing the majority of appointments following booking;
- Demonstrate a lack of co-operation with health care services and/or non-compliance with medical treatment;
- Present with a lack of understanding (or an unwillingness) to learn the needs of their unborn and how pregnancy should progress;
- Are a pregnant child under the age of 13, (see SPB Jersey Children's Sexual Development, consent and risk Procedure);
- Have problematic substance use (including alcohol) (See SPB Jersey Safeguarding Children whose Parents are Problematic Substance (including Alcohol) Users Procedure);
- Signs of serious neglect of self and living conditions;
- Have experienced Maternal Female Genital Mutilation (FGM) and there are concerns about FGM for their unborn baby or baby in the future, (See SPB Jersey FGM Procedure);
- Present with risk of Child Trafficking, Modern Slavery, Forced Marriage, or risk of Honour Based Violence (see SPB Jersey Forced Marriage Procedure, Honour Based Violence Procedure, Child Trafficking and Modern Slavery Procedure);
- Have had previous children removed from their care;
- Have had previous children who experienced abuse, neglect, sustained non-accidental injury or the sudden unexpected death of a child due to safeguarding concerns (see SPB Jersey Recognising Abuse, Neglect and Exploitation Procedure);
- Present with risk of Child Sexual Abuse/Exploitation (see SPB Jersey Child Sexual Exploitation and Child Sexual Abuse in the Family Environment Procedure);
- Have persons in the household/family who pose a risk, or potential risk to children with regard to child abuse, child sexual abuse or exploitation (see SPB Jersey Recognising Signs of Abuse, Neglect and Exploitation Procedure, Child Exploitation Procedure and Child Sexual Abuse (CSA) in the Family Environment Procedure);
- Have a dangerous dog (or significantly poorly cared for animals in the home (see SP Jersey Dangerous Dogs Procedure and VAWG data around poorly cared for animals and links to domestic abuse and child neglect);
- Have a history of violent, criminal behaviours or those who have been/are currently in prison or on probation for similar offences;
- Themselves been subject of a health and development plan (CiN Plan), subject to a Child Protection Plan and/or are a Looked after Child with safeguarding needs of their own (see SPB Jersey Implementing Child Protection Plans Procedure, Children Looked After Living Away from Home with other Families Procedure);
- Hold concerns their baby may suffer or be likely to suffer harm from Fabricated or Induced Illness (FII), (See SPB Jersey Perplexing Presentation and Fabricated and Induced Illness Procedure).
Where an unborn baby has safeguarding needs and may be at risk of significant harm, practitioners must:
- Where there is an immediate risk of harm, call the police on 999;
- Refer to the Children and Families Hub for support (following the the SP JERSEY Children and Young People Safeguarding Referrals Procedure);
- Inform the Health Safeguarding Team;
- In parallel (where required), refer any adult or young person (and with consent) to supportive domestic abuse services (JDAS, FREEDA);
- Raise a safeguarding referral to the Single Point of Referral where the pregnant person is an adult with care and support needs and presents at risk of harm in their own right.
Following referrals, it is important that practitioners:
- Receive a timely response (and/or request outcome if this is not received);
- Agree with the response to their referral;
- Where they have a difference of professional opinion about the outcome of referral, seek further advice with their Designated Safeguarding Leads, and either re-refer with more information or follow the Professional Difference/Escalation Process (see below);
- Practitioners must consider their agreement with any decision-making regarding whether a Pre-Birth Wellbeing Assessment is to be carried out or not, and where they are not in agreement, follow the Professional Difference/Escalation Process (see below).
Where there is curiosity/uncertainty/doubt, practitioners should seek advice from their Designated Safeguarding Lead, from the Health Safeguarding Team, the Safeguarding Midwife Advisor and/or the MASH Decision Maker (See SPB Jersey Child and Young Person Safeguarding Referral Procedure) who can offer advice and support.
Where Children's Social Care decides not to progress a referral and does not undertake a Pre-Birth Wellbeing Assessment, the rationale for this decision must be shared with the referring supportive service. This must be clearly recorded in each agency's files, and there must be a multi-agency agreement with this decision. Any further identification of need requires a re-referral to the Child and Families HUB and other supportive services where required.
Where there are identified health and development needs or safeguarding needs, a Wellbeing Pre-Birth Assessment should commence as soon after a viable pregnancy has been confirmed as possible, (12 - 16 weeks gestation or sooner if required). Where the initial identification of the pregnancy is delayed/concealed, commence as soon as the pregnancy has been identified.
Purpose of a Pre-Birth Wellbeing Assessment
The purpose of a Pre-Birth Wellbeing Assessment is to bring supportive services together to understand prospective parents/carers' views, their needs and their unborn babies' needs and to identify:
- The strengths in their family unit;
- What parents/carers wish to contribute, their ideas and solutions, as working restoratively with parents/carers is likely to increase engagement and lead to positive outcomes;
- Steps which can be taken to improve health outcomes, and where necessary, reduce risk to the baby in utero, at birth and into childhood;
- Where there may be increased risk of sudden unexpected death in infancy (SUDI), the steps parents/carers and practitioners can take to reduce them (see SPB Jersey Multi-Agency Neglect Strategy - SUDI Assessment Tool Kit);
- Their feelings towards their unborn baby and the meaning the baby has for them;
- The support to be offered to meet their needs;
- Understand and agree on the need for support, and if parents/carers are able to work with the support they are offered to make changes to meet their baby's needs;
- Whether they demonstrate sufficient parental capacity;
- How to optimise their home circumstances prior to the birth.
A Pre-Birth Wellbeing Assessment will:
- Be carried out by a qualified children's social worker who will then be the Lead Worker and coordinate the TAC plan of care;
- Incorporate the 8 wellbeing indicators (one of which is the assessment of Safety and Risk);
- Be carried out in partnership with the TAC, which should include the GP, Midwives, Health Visitors, and any specific adult-based services such as Mental Health, Drug and Alcohol Services, Adult Social Work - all of whom must contribute to the Wellbeing assessment in accordance with the JCF Practice Framework;
- Used to identify any specialist parenting assessments which may be required, such as Parenting Assessment Manual (PAM).
A Pre-Birth Wellbeing Assessment will identify:
- Strengths;
- Needs;
- Family history and functioning;
- The needs of fathers/or other significant carers, and/or frequent visitors to the home who are in a caring role;
- Factors likely to change, reasons for this, and whether these are strengths or needs;
- Actions required to reduce risks.
The Pre-Birth Wellbeing Assessment should be completed within 45 days, where the allocated CSW should share this with their manager, and with the prospective parent(s)/carer(s).
The outcome of a Pre-Birth Wellbeing Assessment may recommend a:
- Step down to an EHWP, with the offer of a voluntary Team Around the Child approach;
- The development of a Wellbeing Child in Need Plan (CiN Plan);
- Progression to Pre-Birth Initial Child Protection Conference (ICPC), (for further guidance on the procedures about pre-birth ICPC - see SPB Jersey Safeguarding Core Procedures);
- Along with this, there may be plans to seek legal advice and a legal plan to consider initiating pre-proceedings before birth and/or initiating proceedings at birth.
Practitioners should consider their agreement with the outcomes of the Pre-Birth Wellbeing Assessment. If they disagree, they should seek advice from their Designated Safeguarding Leads and follow the Professional Difference/Escalation Process (see below).
The outcome of a Pre-Birth Wellbeing Assessment should be communicated to parents and the team around the unborn child by 20 weeks gestation to allow time for the plan to be shared with all services and to reduce anxiety and concern for parent(s)/carer(s) around the time of birth.
Pre-Birth Strategy Meeting/Discussion (see SPB Jersey Article 42 Child Protection Enquiries Under the Ministers Duty to Investigate Procedure).
A Pre-Birth Strategy Meeting/Discussion will determine the need for Article 42 Enquiries to commence. It must be called before the calling of an Initial Pre-Birth Child Protection Conference (see SPB Multi-Agency Pre-Birth Flow Chart). Where an unborn child presents with Safeguarding needs following a Pre-Birth Wellbeing Assessment (or at any time safeguarding needs are identified in pregnancy), a Pre-Birth Strategy Meeting/Discussion will be called by children's social care. This should be called by 20 - 24 weeks gestation or earlier if there is a history of premature birth). This is to ensure appropriate multi-agency planning can take place within optimum time-scales of pregnancy (see SPB Jersey Child Protection Conferences Procedure). Noting the time scale for strategy discussion/meetings may be dependent on the date a referral has been made to Children's Social Care.
Practitioners must consider their agreement with the outcomes of Pre-Birth Strategy Discussions/Meetings. If they disagree, they should state this within the discussion/meeting and try to reach an agreement. If this is not possible, seek further advice from their Designated Safeguarding Leads and follow the Professional Difference/Escalation Process (see below).
TAC Pre-Birth ICPC (see SPB Jersey Core Procedures Child Protection Conference Procedure and Implementing Child Protection Plans Procedure).
Where a child has a TAC Plan (this may be a CiN, CP or Looked After Child Plan), certain meetings may have a different focus, for example, there may be the need for a Birth/Discharge Planning Meeting. All meetings follow the JCF Framework of the TAC and are included in one plan for the child and their family. All TAC plans must be shared with the prospective parents/carers.
Where it is not possible to hold a TAC Pre-Birth ICPC before the birth of the baby, children's social care must take the actions required to protect the baby from risk of significant harm at birth and give consideration to convening an ICPC at the earliest opportunity.
Practitioners must consider their agreement with the outcomes of a TAC Pre-Birth ICPC and, if they disagree, state this within the meeting where possible. They should then seek further advice from their Designated Safeguarding Leads and follow the Professional Difference/Escalation Process (see below).
The first pre-birth RCPC should be called before the birth of the baby around 33 - 37 weeks gestation (or 3 months post ICPC, if the initial ICPC was out of this timescale) and thereafter 6 monthly.
Where legal action and legal planning are to be considered. A legal planning meeting should be held as soon as possible to consider initiating action under pre-proceedings and/or initiating care proceedings at birth.
There must be an aim to avoid additional stress for prospective parents/carers in the later stages of pregnancy, where there is the time:
- For parents/carers to obtain their own legal advice;
- For supportive services to commission specialist assessments;
- To work with extended family members through a family group conference;
- Arrange support and service provisions to meet need;
- Where possible, to avoid the need for legal proceedings.
The Public Law Working Party (March 2021) published "Recommendations to achieve best practice in the child protection and family justice systems". This provides national guidance on best practice in decision making at legal planning meetings, the support for families before court proceedings and when making an application to a court in care proceedings. The report recommends local authorities and those who provide maternity services develop protocols setting out the arrangements for the birth at hospital and an agreed period for the baby to remain in hospital to allow an application to be made to court in a timely way: and their family justice board agree protocols providing clarity of expectation and principles under the pre-proceedings phase of the Public Law Outline.
Following Pre-Birth Wellbeing Assessment, where the unborn baby requires a Health and Development Plan (CiN Plan), the lead worker will be the unborn baby's allocated social worker and they will lead on calling a timely TAC (CiN Meeting. The first TAC (CiN) Meeting should be called 10 days after the Pre-Birth Wellbeing Assessment, which determined the unborn child required support under a health and development TAC (CiN) Plan. Where possible, the first meeting should be carried out at 20 - 24 weeks gestation and follow up TAC (CiN) Meetings at least every 4 weeks. The frequency can be increased when the need of the unborn child requires this. Should risk increase during the pre-birth child in need planning period, a strategy meeting will be called, and child protection procedures will be followed.
Where a child has an Early Help Plan and they have identified needs, consideration should be given to calling a Birth Planning Meeting/Discussions.
Where a child has a TAC CiN, CP or Looked After Child Plan the Social Worker will call the CiN, Core or Looked After Child TAC Meeting to specifically discuss Birth Planning before 34 weeks gestation, or earlier if there is a risk of premature birth.
TAC plans for the unborn baby might be to issue proceedings upon birth, and the plan might include separation from parents.
TAC Meeting members should agree on a detailed plan to safeguard the baby, which should include:
- How long the baby will stay in hospital (for example, for babies who may require monitoring for foetal abstinence syndrome);
- How long the mother will remain in hospital;
- Means to reduce the risk of parents/carers seeking to remove the baby from the hospital, where multi-agency and single agency policy and procedures should cover actions which include the consideration for:
- Hospital security;
- Police protection;
- Custom and Immigration Services.
- The plan for the baby upon discharge, and what visits will be made upon discharge and by whom;
- Contingency plans in the event of a sudden change in circumstances, these should include instructions on what to do if the birth happens, at home, out of normal working hours, over the weekend/Bank Holidays and who to contact.
TAC Plans should consider:
- How the mother/prospective parents/carers wish to feed their baby;
- Any medical/pregnancy-related health issues for the mother, prospective parents/carers or baby;
- The supportive services required to meet the needs of the baby if they wish to/or have a sudden home delivery;
- Which practitioners need to be contacted should the baby be born out of hours, with shared contact numbers and a plan for out-of-hours delivery;
- The arrangements for the immediate protection of the baby at birth were required;
- The need for a discharge planning meeting prior to the baby's discharge home from a hospital birth;
- Ensure there are effective arrangements to manage risks identified during the assessment and that the arrangements are detailed within the child's plan;
- Where supervision is required, identifying and naming supervisors;
- The plan for family time in the hospital between the family, siblings and the baby;
- All agencies should receive a copy of the minutes from the TAC meeting discussion, as well as any other relevant agencies that require an understanding of the decision-making at this meeting, for example, GPs;
- The Safeguarding Midwife Advisor should inform midwifery staff of the details of the TAC plan. This may involve liaison with senior midwives on shift at the time and should be documented in the mother's and baby's medical records;
- The Social Worker should inform that the child's TAC plan is up to date on their electronic MOSAIC record and that the child's summary is also updated to reflect the plan, contingency arrangements, and contact details. This is to ensure that the out-of-hours service can ensure the plan is followed. The service should inform the On-Call CSW Duty Team of the outcomes and provide a copy of the Birth Plan.
Other TAC Meetings:
- TAC - Birth Planning - is for practitioners and parents/carers to be clear about their roles and responsibilities with regard to multi-agency working together and/or the actions required to safeguard the baby and support the family following birth (see SPB Jersey Introduction and Practice Guidance on Roles and Responsibilities Procedure). Note: The police do not normally attend Birth Planning Meetings or Discussions. The agreed-upon plan should be shared with the police by the Social Worker so that they can update their records;
- TAC - Discharge Planning Meeting - If at birth the child is subject to an Early Help Wellbeing Plan, then consideration should be given to convening a discharge planning meeting. If at birth a baby has a CiN, CP or Looked After Children Plan, consideration must be given to convening a discharge planning meeting. Decisions not to convene a Discharge Planning Meeting should be recorded by the Lead Worker. The purpose of a TAC discharge planning meeting is to draw up a detailed plan before the baby's discharge home (this may be combined with a core group meeting. (See SPB Jersey Child Protection Conferences Procedure).
The hospital midwives should inform children's social care of the birth of the baby as soon as possible (ideally, the allocated social worker will be notified once the expectant mother is admitted to the hospital in established labour).
Prospective parents/carers should be fully informed and know the TAC plan of care for their child and understand there will be regular liaison between supportive services, CSW and midwifery whilst they and their baby are in hospital and on discharge home.
Midwifery staff should keep records of strengths, needs, and any risks whilst in hospital, as this provides important information for child protection planning or evidence needed for care proceedings.
The police should be informed of the birth of any child on a child protection plan so their records can be updated. The police should create a Notification Case Record.
On the rare occasions legal decisions have been made to initiate care proceedings following birth, all necessary paperwork must be prepared in advance of the birth to prevent any delay. Children's Social Care must keep the Safeguarding Midwife Advisor and maternity staff updated about the timing of any application to the Courts.
Where a Care Order is granted, it is the responsibility of the Children's Social Worker to complete a notification of change form and inform within one working day of the order being granted:
- Police (PPU);
- The Safeguarding Midwife Advisor;
- The Health Safeguarding Team.
Where there is a need for an urgent Discharge Planning Meeting, the lead CSW should call this within 1 working day of the order being granted.
Children's Social Work Business Enablement Team will forward Notification of Change forms to other relevant agencies (on a need-to-know basis) within 1 working day:
- Family Nursing and Home Care;
- Education;
- Health;
- Finance;
- The Independent Reviewing Officer;
- Income Support;
- GP;
- Others - as specific to the case.
All safeguarding partners must have a process in place upon receiving this information and understand their roles and responsibilities to the child who has had an order granted.
Step Down to TAC EHW Plan
Where an EHW Plan or a Health and Development plan is recommended from the outcome of a Pre-Birth Wellbeing Assessment, the CSW should follow recommendations in the CoN around stepping down a case to Early Help.
Prospective parents/carers should be encouraged to identify their preferred Early Help Co-ordinator and, with their consent, be offered targeted support with an identified TAC. TAC meetings then provide a forum for sharing information and to help identify a multi-agency package of support.
TAC meetings should take place as soon as possible post Pre-Birth Wellbeing Assessment, preferably by 26 weeks gestation. TAC meetings should be called monthly until the birth of the baby and thereafter, post-birth, until case closure.
Case Closure Pre-Birth Wellbeing Assessment with continued Universal Service Provision
Where the Pre-Birth Wellbeing Assessment finds there is no need for further support, the case for the unborn baby will be closed by Children's Social Work. The reason for closure is clearly recorded and shared with the multi-agency in writing, with advice to re-refer where there is identification of previously unknown need or immediate concerns for the unborn baby's welfare. All prospective parents/carers are offered a programme of universal health services throughout pregnancy and beyond.
Parents to be with Learning Disability (see SPB Jersey Supporting Parents with Learning Disabilities Procedure and recent research Babies in Care Procedures: What Do We Know About Parents with Learning Disabilities or Difficulties 2024 - looking at 10 aspects which need to be addressed in any TAC Wellbeing Assessment.
Multi-Agency JCF Chronology
A multi-agency JCF chronology is recommended and essential when assessing strengths and needs.
Working with Fathers/Partners
Fathers play an important role during pregnancy and throughout their children's lives. The National Service Framework for Children, Young People and Maternity Services (2004) states:
'The involvement of prospective and new fathers in a child's life is extremely important for maximising the life-long wellbeing and outcomes of the child regardless of whether the father is resident or not. Pregnancy and birth are the first major opportunities to engage fathers in appropriate care and upbringing of children.'
NSPCC learning 2022 states "involving male caregivers can play a crucial part in a child's wellbeing, but they may need education to support them in this role", NSPCC advise they should:
- Be encouraged to attend health care appointments, antenatal appointments and antenatal classes;
- Be involved in assessments, identifying strengths and needs, where practitioners should understand any physical or mental health needs they may have;
- Be asked directly about their life choices, behaviours and any risky behaviours such as their drug and alcohol use, offering them services based on their needs;
- They should be informed of concerns in relation to their children, be consulted on plans, invited to child protection conferences and included in core groups.
Services should ensure they have processes and procedures in place to assess fathers and address their needs. Practitioners may need specific training on how to engage fathers (see SPB Jersey Training). Fathers must be part of assessments, Early Help, CiN plan or Child Protection Plan and should ascertain father's attitude towards the unborn baby, the mother and newborn baby and their thoughts, feelings and expectations about becoming a parent (see SPB Jersey Core Procedures - Assessment Procedure see also The science behind dads | Life as a parent articles & support | NCT).
Partners who are not biological fathers
In a similar way information should be gathered about partner(s)/carer(s) who are in a relationship with the pregnant person but are not the biological father, all prospective parent(s)/carer(s) should be involved in assessment from a strength based perspective and to needs (and risks where necessary) can be identified. This should be based on whether they are living in the family home or not.
For more information about risk factors, see "The myth of invisible men: safeguarding children under 1 from non-accidental injury caused by male carers".
Concealed or Denied Pregnancy
There is an increased risk of serious obstetric and medical complications to the pregnant person and the baby if they do not receive antenatal care or have late or only partial antenatal care.
If a pregnant person is a late booker and has not been receiving antenatal care, then their reasons for not doing so should be explored. They should be supported so they receive antenatal care and are booked in for delivery as soon as practicable. Once reasons are more fully understood, where they present with:
- Wellbeing needs should be offered a TAC EHWA;
- Health and development or safeguarding needs should be referred to the Child and Families HUB for consideration of a Pre-Birth Wellbeing Assessment.
Where a person conceals or denies a pregnancy, and they have not received ante-natal care, and the baby is born either at home or in hospital, this should trigger referral to the Children and Families HUB.
Where a person gives birth in a hospital and they have not received antenatal care, they should not be discharged home until the outcome of the Children and Families HUB referral is known. If there are health and development needs or safeguarding needs, a discharge planning meeting must be convened.
NICE Quality statement 5: Women with no antenatal care
BMC Under-attending free antenatal care is associated with adverse pregnancy outcomes
BMC Understanding delayed access to antenatal care
Failure to Attend Antenatal Appointments
If a pregnant person fails to attend antenatal appointments and cannot be located, information should be shared with maternity services in other neighbouring areas, (this could involve overseas locations and not solely in the UK). Should a pregnant person present at a different hospital from that which had provided their antenatal care seeking assistance / in labour, then the originating hospital maternity services should be contacted and asked to provide relevant information about, any needs or risks that they may have identified.
If a pregnant person disengages from maternity services and Children's Social Care have already commenced a Pre-Birth Wellbeing Assessment, then they should be notified, and consideration taken to safeguard the welfare of the unborn baby (see SPB Jersey Children Moving Into and Out of the Island Procedure).
It is a multi-agency responsibility to make all attempts to re-engage the pregnant person with maternity services in order to ensure the best possible outcomes for both the pregnant person and the baby.
If a referral has been forwarded to children's social care and the decision is made not to undertake a Pre-Birth Wellbeing Assessment and practitioners are initially in agreement with this decision, if when further steps are made to support the pregnant person and they do not engage, a further enquiry should be made to the Children and Families HUB with this further information.
Pregnancy of Young People in Care/Care Leavers
Careful consideration should be given when working with both prospective parents/carers who are looked-after children or care leavers. It is important that practitioners do not make assumptions about a child in care or a care leaver's unborn baby has safeguarding needs, but that there is consideration given to their strengths, needs and risks. Often, children in care and care leavers have less in the way of a supportive family network around them and are likely to require financial support and support with housing.
Where a Pre-Birth Wellbeing Assessment is required for the unborn child, this assessment should not be undertaken by the child in care or care leavers, their allocated personal advisor, or their allocated social worker. The unborn baby's case should be allocated to another CSW to allow them to separately assess the needs of the unborn child from the best interests of the looked-after child/care leaver. This allows objectivity and for the child in care/care leaver to maintain their relationship with their key worker.
If the looked-after child is placed outside of Jersey (Jersey continues to be the Local Authority (LA) with statutory responsibility for them). The Pre-Birth Wellbeing Assessment should be carried out in partnership with the LA in whose area they are residing (dependent on their placement) and the LA with statutory responsibility for them (Jersey). There should be representation from both authorities at ICPCs, RCPCs, birth and discharge planning meetings. Jersey has a statutory responsibility for the person in care. They should take the lead in ensuring the needs of the care leaver are planned for and met-the needs of the baby under the care of the LA where they are born.
Personal advisors play an important role in supporting care leavers, and their ability to form helpful relationships is well evidenced. Assumptions should not be made about their role in identifying the potential risk to babies; there can be a tendency for other practitioners to attribute a greater degree of responsibility for this to personal advisors than should be the case.
Moving into and out of the Island
Where an expectant mother moves between local authority areas, the Pre-Birth Wellbeing Assessment must be undertaken in a consistent manner.
For any pregnant person (other than a child in care as explained above), the local authority in whose area the pregnant person is residing retains responsibility for Pre-Birth Wellbeing Assessment and until completion, where they are:
- Homeless;
- In prison;
- Or they present at a hospital without having previously booked at that hospital and/or having not previously received antenatal care elsewhere.
Multi-Agency Flow Pre-Birth Wellbeing Assessment Flow Chart and Appendix 1.
Training
Practitioners must be supported through training to understand their roles and responsibilities to safeguard the unborn baby. See SPB Training.
Supervision
Practitioners should have access to regular Single Agency Supervision.
Agencies should consider multi-agency reflective supervision where cases are complex, stuck or drifting.
Resolving Professional Difference/Escalation
Professional challenges should be welcomed, and partnership working depends on resolving professional differences and conflicts as soon as possible. Where staff experience professional differences, they must follow the SPB Jersey Escalation Policy and Resolution Pathway Procedure.
Last Updated: September 19, 2025
v91